
Why Over-the-Counter Birth Control?
Oral contraceptives have been around since 1960, and their risks and safety profiles have been well-studied throughout the years. According to the Guttmacher Institute, unplanned pregnancies account for 45% of all pregnancies in the US. Furthermore, nearly one-third of individuals who have tried to obtain a prescription for hormonal contraception report difficulty doing so. Polling from Data for Progress in 2022 shows that the majority of Americans, regardless of political affiliation, support making birth control available over the counter.
The push for over-the-counter (OTC) birth control is driven by the need to expand access to safe and effective contraception. Research shows that women and teens who are uninsured, currently use a less effective contraceptive method, or tried to get a birth control prescription in the past year are more likely to use OTC birth control. Being able to acquire birth control over the counter would especially benefit marginalized communities and individuals who face healthcare barriers, such as transportation, cost, language, and lack of physician access.
Over 100 countries worldwide have approved OTC birth control options, but as of April 2023 the United States is not one of them. The American College of Obstetricians and Gynecologists, American Medical Association, and American Academy of Family Physicians concur that oral contraceptives should be approved for OTC use. In June 2022, the AMA urged the FDA to approve an OTC contraceptive method with no age restriction.
How Do We Get an OTC Birth Control Option?
In order for a drug to be approved for OTC use by the FDA, certain criteria must first be met. The drug must be safe, treat a condition that patients can diagnose by themselves, have a low potential for abuse or misuse, and be available for use without supervision of a healthcare provider. Oral contraception checks all of these boxes.
The next step is having a pharmaceutical company manufacture a product that can be FDA-approved for OTC use. HRA Pharma, a French pharmaceutical company acquired by Perrigo, is working with Ibis Reproductive Health to bring the product Opill to the US market.
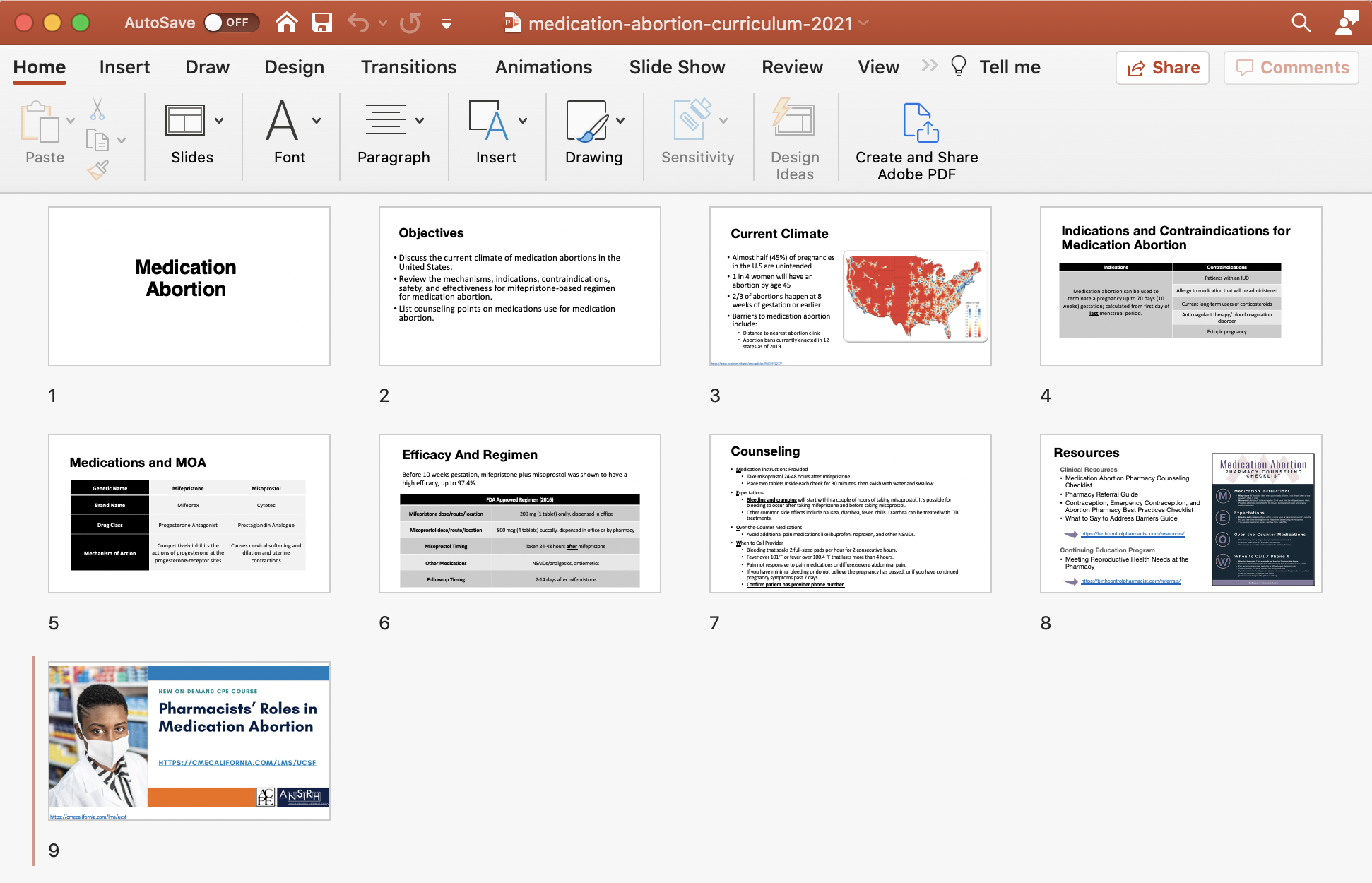
What is Opill?
Opill, the product manufactured by HRA Pharma, is a progestin-only pill for which Ibis and HRA Pharma are seeking FDA approval. If approved, Opill will become the first oral contraceptive available over the counter in the US.
There are two types of oral contraceptives: combination pills (containing both estrogen and progestin) and progestin-only pills. Progestin is a form of the endogenous hormone progesterone, and it plays a key role in the menstrual cycle. Progestin, along with other hormones, helps start and stop the menstrual cycle. Low progestin levels in the body cause shedding of the uterus lining, signaling the start of menstrual bleeding. High progestin levels in the body (i.e., when you’re taking a progestin-only pill) cause the cervical mucus to thicken, making it harder for sperm to enter the uterus and fertilize an egg.
Progestin-only pills are deemed safer than combination oral contraceptives. Due to estrogen’s pro-coagulatory nature, combination oral contraceptives carry the risk of adverse effects related to thromboembolism, or blood clotting. The lack of estrogen in progestin-only pills means it is preferred in individuals who smoke, have high blood pressure, experience migraines with aura, or are otherwise at risk of blood clots.
On July 11, 2022, HRA Pharma submitted their application for FDA approval of Opill. The FDA review process is expected to take about 10 months. Opill has been approved for prescriptive use since 1973, so its safety data has stood the test of time. Traditionally, progestin-only pills must be taken at the same time each day, with only a three-hour window of tolerance before requiring back-up contraception (e.g., male condom). However, recent research has found that there is a larger margin of error than previously believed. Because different progestin-only pills contain different types of progestin, they act on the body through different mechanisms. Thus, some progestin-only pills (including norgestrel-only formulations such as Opill) may not adhere to the strict three-hour window of administration.
When Can We Expect a Decision from the FDA?
Previously, the FDA planned to hold a joint meeting on November 18, 2022 with the Nonprescription Drugs Advisory Committee (NDAC) and the Obstetrics, Reproductive, and Urologic Drugs Advisory Committee (ORUDAC) to review HRA Pharma’s Opill application. This joint meeting was put off indefinitely until March 28th of this year, when the FDA announced that it has rescheduled the advisory committee meeting for May 9-10, 2023. May 9th is also Free the Pill Day, which celebrates the anniversary of the first birth control pill in the US becoming FDA-approved in 1960.
Currently, the nationwide movement involving pharmacists prescribing hormonal contraceptives helps circumvent healthcare barriers and make birth control more accessible. The approval of Opill would further aid in the removal of these barriers and see a monumental expansion of contraceptive access, bringing us one step closer to providing patients with the healthcare they deserve. We look forward to the FDA’s decision as May 2023 draws near.
References
- Abrams A. First U.S. application for over-the-counter birth control pill. Time. https://time.com/6195124/birth-control-pill-over-the-counter-fda/. Published July 14, 2022. Accessed April 13, 2023.
- Data For Progress. Files For Progress. Data For Progress. https://www.filesforprogress.org/datasets/2022/5/dfp_22_cai_tabs.pdf. Published 2022. Accessed April 14, 2023.
- Finer L, Zolna M. Declines in unintended pregnancy in the United States. 2008–2011, New England Journal of Medicine, 2016, 374(9):843–852, doi:10.1056/NEJMsa1506575.
- Grindlay K, Grossman D. Interest in Over-the-Counter Access to a Progestin-Only Pill among Women in the United States. Womens Health Issues. 2018;28(2):144-151. doi:10.1016/j.whi.2017.11.006
- Grindlay K, Grossman D. Prescription Birth Control Access Among U.S. Women at Risk of Unintended Pregnancy. J Womens Health (Larchmt). 2016;25(3):249-254. doi:10.1089/jwh.2015.5312
- Wollum A, Zuniga C, Blanchard K, Teal S. A commentary on progestin-only pills and the “three-hour window” guidelines: Timing of ingestion and mechanisms of action [published online ahead of print, 2023 Feb 19]. Contraception. 2023;109978. doi:10.1016/j.contraception.2023.109978.
Photo credit: Image from FreethePill.org
 About the Author
About the Author
Matissa Peng, Pharm.D Candidate, is a 3rd-year student pharmacist in the Class of 2023 at the University of the Pacific Thomas J. Long School of Pharmacy. Matissa completed an elective APPE rotation with Birth Control Pharmacist.


 About the Author
About the Author
 About the Author
About the Author
 About the Author
About the Author The current recommended dosing is one tablet by mouth daily in the order provided by the blister pack for 28 days. The blister pack contains twenty-four active ingredient pills followed by four inert pills. The first active tablet should be taken on the first day of the menstrual cycle daily at the same time every day. If Nextstellis is not taken on the first day of menses an additional non-hormonal contraceptive method should be used for the first seven days.1 Nextstellis can be taken with or without food.2
The current recommended dosing is one tablet by mouth daily in the order provided by the blister pack for 28 days. The blister pack contains twenty-four active ingredient pills followed by four inert pills. The first active tablet should be taken on the first day of the menstrual cycle daily at the same time every day. If Nextstellis is not taken on the first day of menses an additional non-hormonal contraceptive method should be used for the first seven days.1 Nextstellis can be taken with or without food.2 Athina Herrera Ng, PharmD Candidate 2023, is currently in her third year of pharmacy school at Midwestern University College of Pharmacy-Downers Grove. She holds the Event Chair position for Pharmacy and Pediatrics and is invested in learning more about women and children’s health. She is passionate about creating art in her free time as well as helping others heal through expressive therapy.
Athina Herrera Ng, PharmD Candidate 2023, is currently in her third year of pharmacy school at Midwestern University College of Pharmacy-Downers Grove. She holds the Event Chair position for Pharmacy and Pediatrics and is invested in learning more about women and children’s health. She is passionate about creating art in her free time as well as helping others heal through expressive therapy. Kayla Mitzel, PharmD Candidate 2023, is currently in her second year of pharmacy school at Midwestern University College of Pharmacy – Downers Grove. She is serving as the President Elect for APhA-ASP, and the Member at Large for CPNP. Her hobbies include running and biking.
Kayla Mitzel, PharmD Candidate 2023, is currently in her second year of pharmacy school at Midwestern University College of Pharmacy – Downers Grove. She is serving as the President Elect for APhA-ASP, and the Member at Large for CPNP. Her hobbies include running and biking. 





 Samantha Thompson, PharmD Candidate is a pharmacy student in the Class of 2023 at University of California San Diego Skaggs School of Pharmacy and Pharmaceutical Sciences. Samantha completed a summer internship with Birth Control Pharmacist.
Samantha Thompson, PharmD Candidate is a pharmacy student in the Class of 2023 at University of California San Diego Skaggs School of Pharmacy and Pharmaceutical Sciences. Samantha completed a summer internship with Birth Control Pharmacist.